Toronto’s healthcare landscape is shifting rapidly, and not everyone’s convinced it’s for the better. A concerning report published yesterday suggests Ontario may be redirecting essential public health dollars to fund private clinics, a move that’s causing particular anxiety in urban centers like Toronto where healthcare demands are already stretched thin.
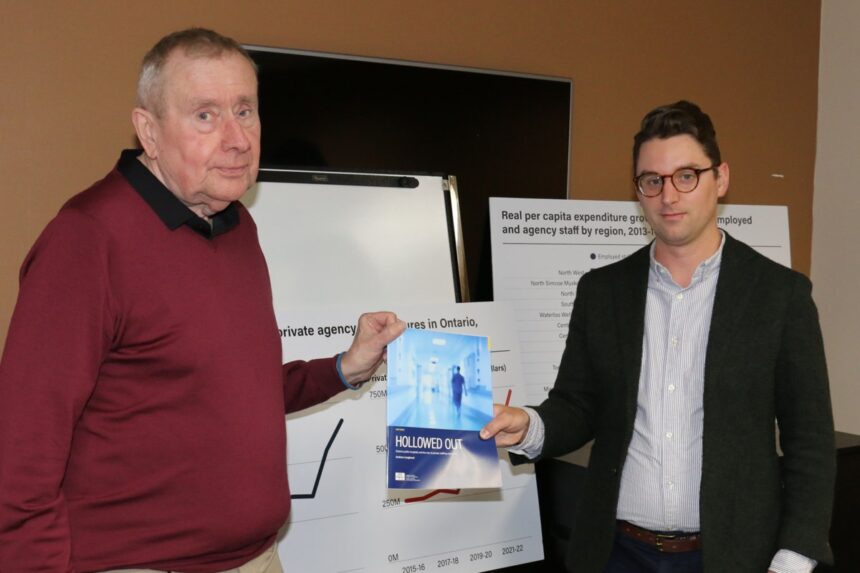
The Ontario Health Coalition released findings indicating the province has been quietly reallocating funds from public hospitals and health services toward privately-operated facilities. According to their analysis, approximately $521 million in public funding has been directed to private surgical and diagnostic clinics over the past fiscal year.
“What we’re seeing is essentially robbing Peter to pay Paul, but both Peter and Paul are the same Ontario taxpayers,” says Dr. Maya Patel, a Toronto-based healthcare policy analyst I spoke with yesterday. “The difference is that public funds going to private clinics often mean higher costs overall and fewer accountability measures.”
For Toronto residents, this shift raises particular concerns. Our city’s hospitals already face significant wait times for many procedures, with some patients waiting 6-8 months for non-emergency surgeries at major facilities like Toronto General and St. Michael’s Hospital.
When I visited Toronto Western Hospital last week for an unrelated story, I noticed the packed waiting rooms and spoke with Sandra Thompson, a nurse of 17 years. “We’re already working with limited resources,” Thompson explained. “If funding gets diverted elsewhere, I honestly don’t know how we’ll manage the patient load we already have.”
The provincial government maintains that expanding private delivery options creates more healthcare access points and will ultimately reduce wait times across the system. Health Minister Sylvia Jones has repeatedly stated that “patients don’t care where they receive care, as long as it’s timely, high-quality, and covered by OHIP.”
However, critics point to troubling patterns in other jurisdictions that have pursued similar models. A recent Canadian Medical Association study found that private clinics typically focus on simpler, more profitable procedures while leaving more complex cases to the public system, potentially creating a two-tier healthcare reality.
Toronto City Councillor Joe Cressy expressed concern about the potential impact on the city’s most vulnerable populations. “In a diverse urban environment like Toronto, we need to ensure healthcare access remains equitable. When public dollars flow to private delivery models, we often see service clustering in higher-income neighborhoods.”
The implications for Toronto’s downtown hospitals could be significant. Michael Garron Hospital in East York has already reported a 3.2% reduction in operating budget compared to projected needs, according to internal documents obtained through freedom of information requests.
Perhaps most concerning for Toronto residents is the potential impact on emergency care. While private clinics rarely offer emergency services, the reallocation of resources could further strain emergency departments in the city’s public hospitals, which already face average wait times exceeding provincial targets by 40%.
For Toronto’s business community, the healthcare funding shift presents mixed opinions. The Toronto Board of Trade has cautiously supported exploring alternative delivery models, while emphasizing that any changes must maintain universal access regardless of ability to pay.
“Healthcare is fundamentally both a social and economic issue for Toronto,” notes Deborah Wilson, an economist with the University of Toronto. “Our city’s productivity and competitive advantage depend partly on having a healthy workforce with reliable access to care.”
During a walk through Kensington Market yesterday afternoon, I stopped to chat with several small business owners about the healthcare funding news. Most expressed worry about what this might mean for their employees’ access to care.
“I rely on the public system for my family and my staff,” said Marco Bonetti, who runs a small Italian deli. “If that system gets weakened because money’s going elsewhere, what happens to us? We can’t afford private options.”
As this story continues to develop, Toronto residents should watch closely for how these funding decisions might affect local healthcare access. The ultimate impact will likely be felt most acutely in emergency rooms, specialist wait times, and potentially in growing disparities between healthcare availability in different parts of the city.
For now, healthcare advocates are calling for greater transparency around how and where healthcare dollars are being allocated. The Ontario Health Coalition has requested a full public accounting of all funds redirected from public institutions to private healthcare providers.
As I’ve covered Toronto’s healthcare system over the years, one thing remains clear: changes to funding models rarely affect all communities equally. The question Toronto faces now is whether this potential reallocation will actually improve care access or simply create new inequities in a system already under considerable strain.